Evidence is mounting that opioid pain medication may have played a role in the death of pop legend Prince. While the medical examiner hasn’t yet released the results of the autopsy and toxicology tests in this case, opioid overdose in middle age is all too common.
In 2013 and 2014, according to the The Centers for Disease Control and Prevention, people ages 45 to 64 accounted for more than 40 percent of all deaths from drug overdose. Prince died on April 21 at his home and music studio Paisley Park in Minneapolis. He was 57.
Experts say there are a number of scenarios that increase risk of overdose, which is often accidental, for people over 55. Imagine you are in that age group and you injured your shoulder a while back. It just hasn’t gotten better, so you take prescription painkillers — an opioid like OxyContin — to help with the pain. Let’s say you’ve been taking it for a couple of years. Your body has built up a tolerance to the drug, and now, you need to change it up to get the same amount of relief. When it comes to the potential for overdose, said Boston Medical Center epidemiologist Traci Green, this is one of the most dangerous crossroads.
“We oftentimes see that the dose will increase with an individual over time or they might rotate or switch to another medication to experience pain relief. And so, at each rotation or change, there’s a risk [of accidental overdose] because you’re moving from one drug to another,” she said.
Your body might not be used to that high dose, she said, or that different medication. She continued: Let’s say you also suffer from anxiety. Benzodiazepines can help with that. But taking opioids and benzodiazepines, or “benzos,” together is a dangerous combination.
“There are wonderful medications used for treating anxiety,” she said, but there’s a different calculus when they are taken with opioids.
“One opioid plus one benzo doesn’t equal the effect of two in the individual,” Green said. “It’s like one plus one equals four, or six.”
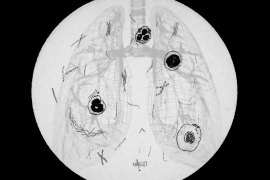
Opioids can depress the body’s drive to breathe and so can benzodiazepines. Combine them and that effect mounts. You could stop breathing and never wake up. And lots of people are taking these drugs in combination. In fact, people in their mid-40s to mid-60s are more likely than any other group to be prescribed opioids with benzodiazepines, according to the National Center for Health Statistics.
“It is indeed a demographic to keep an eye on,” Green said, partly because of another risk factor. People in this older age range may be likely to live alone or be otherwise isolated — maybe from divorce or because their kids have moved out.
So, Green said, “If something happens, if no one’s there to revive you, then you’re more likely to die of that experience.”
University of Rhode Island pharmacy professor Jeffrey Bratberg said the way people in this age group tend to take drugs is also putting them at higher risk.
“They’re taking longer-acting opioids,” he said. “They’re taking doses that, at certain thresholds, are associated with increased overdose death.”
Also, Bratberg said, they’re more likely to have chronic health conditions that put them at higher risk of respiratory depression.
Medical conditions like chronic obstructive pulmonary disease or even the flu can amplify opioids’ ability to depress breathing. And some percentage of these drug users, he said, will develop a substance use disorder.
So why are doctors prescribing so much, in such combinations? Bratberg said it’s how the physicians were trained.
“If you’re a primary care prescriber and your patients are doing OK, maybe you’re just not thinking about that,” he said. “Plus there’s difficulty in telling the person whose pain may be controlled by opioids, and their anxiety may be controlled by benzodiazepines, to say, ‘Now we’re going to taper you off because this is harmful.’ ”
So millions of people are on opioids — most of them over 45 — and that means some are at risk of overdose. Bratberg said we should be educating patients and doctors.
“We’re really making a push nationally and regionally to educate prescribers about those risks, and to use tools available to warn folks about that.”
Tools that help lower the risk include naloxone, the overdose rescue drug. There’s also medication, such as buprenorphine or methadone, to assist people who have become addicted to painkillers to stop their use safely. In essence, those drugs keep a low level of opioids in the system to keep someone from going into withdrawal without getting them high.
This story is part of NPR’s reporting partnership with local member stations and Kaiser Health News.