Alarms go off so frequently in emergency rooms, doctors barely notice. And then a colleague is wheeled in on a gurney, clinging to life, and that alarm becomes a deafening wake-up call.
For Dr. Kip Wenger, that colleague, a 33-year-old physician, was also his friend.
Wenger is regional medical director for TeamHealth, one of the country’s largest emergency room staffing companies, based in Knoxville, Tenn.
“It’s devastating,” he said. “This is a young, healthy person who has everything in the world ahead of them.” His friend had confided in a few co-workers about recent relationship struggles, but none of that had affected her work.
The medical profession relies on the premise that doctors and medical staff, like highly trained endurance athletes, are conditioned to clock long hours, ignoring fatigue and the emotional toll of their work.
But, for many in the profession, that day-in-day-out stress can lead to crippling depression. It’s one reason doctors are far more likely than the general population to die by suicide.
A particular danger for doctors trying to fend off suicidal urges is that they know exactly how to end their own lives and they often have easy access to the means.
Wenger remembered his friend and colleague as the confident professional with whom he’d worked in emergency rooms all over Knoxville — including the one where she died. That day three years ago still makes no sense to him.
“She was very strong-willed, strong-minded, an independent, young, female physician,” said emergency doctor Betsy Hull, a close friend. “I don’t think any of us had any idea that she was struggling as much personally as she was for those several months.”
That day she became part of a grim set of statistics.
A Harsh Reality
An estimated 300 to 400 doctors kill themselves each year, and the suicide rate is more than double that of the general population, according to a review of 10 years of literature on the subject presented at the American Psychiatry Association annual meeting in May.
For TeamHealth, the young woman’s death in 2015 sparked some deep soul-searching.
“A few of these things happened that were just so sobering,” said TeamHealth co-founder Dr. Lynn Massingale. “People don’t stab themselves to death. Young people don’t stab themselves to death.”
It’s been an uncomfortable topic to address. A 2018 study from Mayo Clinic finds disenchanted doctors are more likely to make mistakes.
But TeamHealth held listening sessions and realized that burnout was rampant. To start, they began encouraging doctors to work less. Massingale said the company average is now close to 40 hours a week — though there’s no avoiding nights and weekends in the ER.
The company also started a new protocol for one of the most stressful times in a physician’s career: when doctors are sued. The company then pairs them with someone who has been there.
“We can’t change the facts. We’re not coaching you to change your memory,” Massingale said. “But we can help you deal with the stress of that.”
And TeamHealth is trying to reduce some bureaucratic headaches. A significant portion of the required corporate training has been deemed optional. And the company began spending millions of dollars a year to hire scribes — staff members who follow around ER physicians and enter information into sometimes finicky electronic health records.
Technology has become a real source of stress in a career that comes with lots to worry about, even beyond dealing with patients.
Dr. Jeffrey Zurosky, who is an ER director at Parkwest Medical Center in Knoxville, said he’s concerned for his youngest doctors who start out with a mountain of med school debt, eager to pick up as many shifts as possible.
“I tell them: Be balanced. Don’t overwork yourself. Spend time with your family. Stay married, if you can,” Zurosky said.
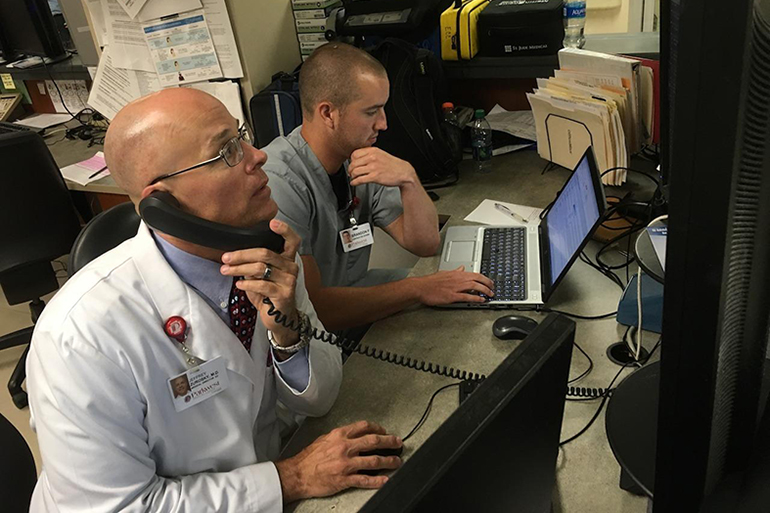
Dr. Jeff Zurosky (left) calls to order a test for a patient as his scribe, Brandon, fills out the patient’s electronic health record.(BLAKE FARMER/WPLN)
Yet to some in the medical community, the problem is far more fundamental than “burnout.” Pam Wible doesn’t even like the term, since it puts the burden on physicians, as if they just have to find a way to cope. The family practitioner from Eugene, Ore., sees it all starting in medical schools. Entrenched ideals, like muscling through long hours on little sleep, are hard to break. Wible calls it abuse.
“These people who have been previously abused are now the teachers,” she said. “They’re teaching the next generation of doctors.”
Too Close To Call For Help
And when physicians do want help, the industry makes it especially difficult. Wible said they can’t go see a psychiatrist without jeopardizing their medical license.
“I know a lot of them,” Wible said. “They’re having to sneak out of town, pay cash and use a fake name to do it. Why are we putting these people in such a situation?”
Wible has collected more than 900 stories of doctor suicides and set up an anonymous help line. She has inspired more physicians to share their experiences, such as an emergency doctor licensed in Ohio.
“You don’t focus on the 99 you save,” that ER doctor said. “You end up focusing on the one that you lose.”
The one he lost was 19 years old and came in with the flu, but tests didn’t show anything unusual. He sent her home. She returned in cardiac arrest. When he found out she died, he went to a dark place — despite no history of depression.
“Like all doctors, you put that Superman cape on and you think you can get through it,” he said.
The family filed a complaint. And being told he might lose his job pushed him over the edge. He swallowed a lethal overdose. But the police found him, and got him to a hospital where he had to be revived.
This ER doc had treated untold numbers of suicidal patients but never saw himself in their place.
“I didn’t know I was at higher risk of suicide than the average person,” he said.
Kaiser Health News and NPR are not naming this doctor because his story could affect his future career. But he said he wishes he could speak more freely, thinking it might encourage physicians to seek help sooner than he did.
This story is part of a partnership that includes Nashville Public Radio, NPR and Kaiser Health News.







