The adoption of electronic health records by community doctors helped drive down health costs, a study published Monday in the Annals of Internal Medicine reported.
Previous studies, many dealing with academic teaching hospitals, have yielded mixed results about the effects electronic health records (EHRs) have had and have drawn concerns over the adoption of health information technology. Federal officials are encouraging the implementation of such systems, arguing that it will help curb the rise in health spending by eliminating duplication of services and medical errors.
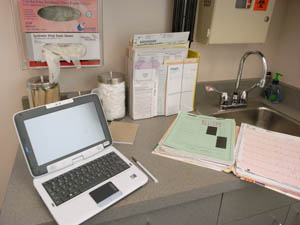
This study, however, is the largest to assess the impact EHRs have in community-based settings, including in private practices and community hospital care.
In the study, researchers analyzed and compared insurance claims data for patient care at three Massachusetts communities that adopted EHRs to six that did not. They found that outpatient spending did not rise as fast in the communities that adopted EHRs as it did in the other six. The difference in cost-growth between the two groups was about 3 percent.
“There’s a lot of anecdotal concern that EHRs are going to drive up the cost of health care. The fact that we didn’t find that is good news,” said Julia Adler-Milstein, an assistant professor at the University of Michigan School of Public Health and the study’s lead author.
The researchers, who analyzed insurance claims data from January 2005 to June 2009, found significant savings in outpatient radiology testing. Adler-Milstein and her colleagues, however, did not find any significant savings relating to outpatient pharmacy or laboratory care, inpatient care and the total cost of care.
“It is significant because we’re looking to control the cost of delivering health care in our country. It’s a huge issue for companies, the government, and individuals. Anything that can help control the cost is going to be a good thing,” said Dr. Glen Stream, the board chair for the American Academy of Family Physicians. He added, however, that the savings from adopting electronic health records may have be even greater if researchers were to analyze more recent insurance claims.
Adler-Milstein and her colleagues plan to do just that to get a better assessment. The researchers looked at data on how EHRs affected these practices’ costs only up to 18 months after implementation of them, she said. “We don’t know if it continued to perform in that way,” Adler-Milstein said, but she suspects the savings will continue.
Chantal Worzala, the director of policy at the American Hospital Association, added that the study showed three important aspects to making digital health records more cost efficient: financial assistance for the health care providers to buy and set up the systems, technical support to help implementation of them, and an efficient infrastructure for data exchange. “When you have all of those things, we’re getting some positive results,” she added.
The study was part of an ongoing project of the Massachusetts eHealth Collaborative, a nonprofit corporation that offers support to health care providers with implementing electronic health records.