Medicaid patients in traditional fee-for-service care get some services at two to three times the frequency of those who are in managed care, especially HMOs, a preliminary report from state officials suggests. But it doesn’t answer the essential question: Is that good or bad?
In the hurried draft, produced under pressure with unverified data, Florida’s Agency for Health Care Administration compares the rate of services that some Medicaid patients with chronic diseases receive in managed-care-organizations with those who use the traditional fee-for-service system, called MediPass.
The draft report suggests that the rate of services for Medicaid patients in all types of managed-care organizations, regardless of how they’re paid, is lower than in MediPass.
It appears to bolster arguments for the importance of coordination of care for patients who have chronic diseases.
This holds true in both the “Reform” counties Duval (in the northeastern part of the state), Broward (the Ft. Lauderdale area) and three small ones and in the rest of the state. In Reform counties, virtually all Medicaid recipients must be enrolled in managed care.
The Florida legislature faces a vote next week on whether to start taking that Medicaid Reform model statewide a move that many see as necessary to balance the budget.
“This absolutely supports all our arguments,” said Michael Garner, president and CEO of Florida Association of Health Plans. He called the difference in rates of use “dramatic.”
“MediPass is not coordinated, has overutilization, and leads to rampant fraud and abuse,” Garner said. “It’s exactly what we’ve been saying.”
But the report is a Rohrshach test. Critics of Medicaid Reform expansion say the report demonstrates that patients in managed care plans may have difficulties getting access to needed services.
‘Taking this data at face value, cringing in the process, it`s clear that the level of access to care is significantly greater in MediPass than in Medicaid HMOs (both Reform and non-Reform),” said Greg Mellowe, policy director for Florida CHAIN.
It’s unwise to throw around charges of over-utilization in Medipass, he said, given that the patients who are being counted have serious chronic diseases. He pointed to the example of patients with hypertension: those in Medipass had 2.6 services a month versus 1.2 for patients in Reform HMOs.
“Remember, that includes all medical services,” he said: doctor visits, hospital stays, emergency care, pharmacy use and non-emergency transportation. “All other things being equal, under-utilization by HMOs seems the much more reasonable conclusion.”
Health-care consultant Brady Augustine of Tallahassee, who specializes in Medicaid issues, said it’s possible that the data reflect difficulty in receiving care, but another factor is important: “case mix.” In general, he said, patients who are the sickest tend not to be enrolled in HMOs.
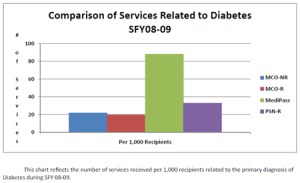
The difference in service levels jumps out in the chart (where MCO stands for managed-care organization, R stands for Reform county, NR stands for non-Reform and PSN stands for provider-service networks, which have been paid under a fee-for-service arrangement in the Reform counties.)
Chart 5 indicates that diabetics in the non-managed system, MediPass, received more than 80 services per 1,000 patients, while the rate of services in managed-care organizations was only a fraction of that.
Consultant Augustine notes that performance measures as reported by independent agencies, listed at http://www.FloridaHealthFinder.gov, show HMOs scoring slightly lower on diabetes preventive care than the provider service networks.
“HMOs probably have fewer recipients who need diabetic care but for those that they do manage, they do not perform as well as their PSN counterparts,” he said.
While the data in the draft report need refinement, he said, at least the report “appears to show that managed care plans are getting their data in to the system.”
To the health plans, it’s about time they got credit for that. “We continue to hear advocates screaming that encounter data do not exist,” Garner said. “It’s not true; it’s simply a misrepresentation.”
Plans are required under their contracts with the state to reports the encounters, and AHCA is required by law to validate the data.
AHCA spokeswoman Tiffany Vause stressed that the agency created the preliminary analysis at the request of a legislator and that it “is NOT conclusive.” She said AHCA is working to validate the data so that they can be used to make policy decisions.






