The Kaiser Health News story and data on Medicare’s quality payment programs are based on data from the Centers for Medicare & Medicaid Services (CMS) containing the Hospital Value-Based Purchasing and Readmissions Reduction Program adjustment factors for individual hospitals.
The Value-Based Purchasing payments for the 2014 federal fiscal year are determined by how hospitals scored on three sets of measures. The first are 13 “measures of timely and effective care” also known as “process” measures. These rate how often hospitals adhered to these clinical guidelines:
Averting Blood Clots in Heart Attack Patients. Percent of heart attack patients given medication to avert blood clots within 30 minutes of arrival at the hospital.
Quick Response to Heart Attacks. Percent of heart attack patients given percutaneous coronary interventions within 90 minutes of arrival.
Discharge Instructions. Percent of heart failure patients given instructions upon discharge about how to take care of themselves.
Taking Blood Cultures. Percent of pneumonia patients who had a blood culture taken before they were given antibiotics.
Correct Antibiotic Selection for Pneumonia Patients. Percent of pneumonia patients that received the correct kind of antibiotics.
Prompt Antibiotic Treatment. Percent of patients that received an antibiotic within an hour of surgery.
Correct Antibiotic Selection for Surgical Patients Percent of surgical patients that received the correct kind of antibiotic.
Prompt Cessation of Antibiotics. Percent of patients who had their antibiotics stopped within 24 hours of surgery.
Controlling Blood Sugar. Percent of heart surgery patients who had their blood sugar kept under control after an operation.
Beta Blockers for Surgery Patients. Percent of heart surgery patients already taking beta blockers who were given a beta blocker just before and after surgery.
Averting Blood Clots in Surgery Patients. Percent of surgery patients who received an appropriate treatment to prevent blood clots.
Prompt Cessation of Blood Clot Treatment. Percent of surgery patients who received anti-blood clot treatment within 24 hours before to 24 hours after the operation.
Averting Catheter Infections. Percent of patients with a urinary catheter where it was removed within 48 hours after surgery.
The second set of eight measures is culled from surveys of patients who had recently left the hospital. These are frequently called “patient experience” or “patient satisfaction” measures. For these measures, Medicare only looked at the percent of patients who said they “always” had a favorable experience in these areas:
* How well nurses communicated with patients.
* How well doctors communicated with patients.
* How responsive hospital staff were to patients’ needs.
* How well caregivers managed patients’ pain.
* How well caregivers explained medication to patients before giving it to them.
* How clean and quiet the hospital room and hall were.
* How often caregivers explained to patients how to take care of themselves after discharge.
* How the hospital stay rated overall.
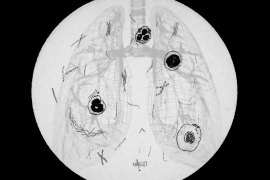
The third area that was evaluated was mortality rates among Medicare patients admitted for heart attack, heart failure or pneumonia. For each, Medicare determined a hospital’s death rate for patients who died while in the hospital or within 30 days after leaving. Medicare adjusted these rates to take into account how sick the patients were.
In calculating death rates, Medicare looked at patients admitted from July 2011 through June 2012, and compared those rates with how the hospitals performed between July 2009 and June 2010. For the clinical and patient satisfaction measures, Medicare assessed hospital performance from April 2012 through December 2012, and compared them with scores during the same months in 2010.
Hospitals with too few cases and certain specialty hospitals, such as psychiatric, long-term care, rehabilitation and cancer hospitals, are exempted from the programs. Medicare also exempted Maryland hospitals from the program because that state has its own payment arrangement with the federal government. Also exempted are Puerto Rico hospitals.
For this year, the process measures account for 45 percent of a hospital’s score, the patient satisfaction measures account for 30 percent and the mortality rates for 25 percent. Medicare calculated a score for both how a hospital did compared to its peers and for how much it improved its own performance over time. Whichever score was higher in each area was the one used to calculate its payment factor.
Hospitals stood to lose or gain up to 1.25 percent of their regular Medicare reimbursements. The amount of money at stake increases incrementally over the next three years to reach 2 percent of payments. Medicare lists and explains its measures.
For the readmissions program, CMS calculated an excess readmission rate for patients who first went into the hospital for three conditions: heart failure, heart attack and pneumonia. The agency based the rate on discharges occurring from July 1, 2009, through June 30, 2012. CMS took into account the severity of illness of each hospital’s patients in estimating what the hospital’s readmission rate should have been given the national averages. If a hospital had fewer than 25 cases for heart failure, heart attack or pneumonia, CMS did not include that condition in its analysis, but hospitals could still receive a penalty if they had 25 cases or more in one of the other conditions. CMS publishes the penalty as an adjustment factor.
The CMS data do not include readmission of patients who are in private Medicare Advantage insurance plans. For the second year of the program, which began with the fiscal year starting Oct. 1, CMS changed its calculations to exclude readmissions that were planned by medical professionals at the time of the patient’s original discharge. CMS originally published the readmissions adjustments in August and then updated them with minor corrections in September. The maximum readmission penalty this year is a 2 percent payment reduction.
To enact the penalties, CMS has created adjustment factors for both the value-based purchasing and readmission reduction programs. The adjustment factor is a multiplier CMS applies to Medicare payments to cover each patient’s stay during the fiscal year beginning in October 2013. The way it works is that a hospital with a value-based purchasing adjustment factor of 0.9945, for example, would be paid 99.45 percent of what Medicare usually reimburses for each service. Thus, if Medicare normally paid the hospital $10,000 for a knee replacement, it would instead pay the hospital $9,945.
CMS has assigned an adjustment factor to each hospital that qualifies for inclusion in the value-based purchasing program, and another factor for each hospital in the readmission reductions program. The factor is applied to all hospital payments for each Medicare patient who is admitted. The factor is not applied to additional Medicare payments for capital expenses, the cost of teaching residents and for treating large numbers of low-income patients.
In the interests of clarity, Kaiser Health News has expressed adjustment factors as a percentage change in payment. Thus, in the previous example, the hospital with an adjustment factor of 0.9945 would be receiving a penalty of 0.55 percent.
KHN excluded from its charts and calculations several dozen hospitals that are not on the government’s list of institutions currently certified to accept Medicare patients but nonetheless are listed by CMS as receiving bonuses or penalties. Most of these hospitals were in operation in 2012, the period where Medicare was measuring them, but closed, merged or converted to outpatient facilities afterward. Because these hospitals were excluded, KHN’s aggregate counts and calculations may be slightly different from CMS’s official numbers and from prior KHN stories and charts, which included closed, merged and converted hospitals.
In some instances, Medicare included a hospital for a given year of one program but not for the other. KHN’s charts and graphics note instances where a hospital was not rated with a [1]. Often, this was because a hospital lacked enough of a particular type of cases that year for Medicare to evaluate. When a hospital was omitted from one or both years of a program, the change in bonus or penalty could not be calculated; those instances are noted with a [2].
Sources:
– Readmission Adjustment Factors for 2013 Fiscal Year
– Readmission Adjustment Factors for 2014 Fiscal Year
– Value-Based Purchasing Adjustment Factors for 2013 Fiscal Year
– Value-Based Purchasing Adjustment Factors for 2014 Fiscal Year (Table 16B)
Read more:
– Nearly 1,500 Hospitals Penalized Under Medicare Program Rating Quality
– Data For Individual Hospitals (interactive chart)