SAN DIEGO — Alton Rodgers had just come in from gardening when he suddenly blacked out and collapsed on the floor. The 89-year-old Kentucky native spent about 10 days at Palomar Hospital, where doctors told him a build-up of fluid around his heart was the culprit.
Now, shortly after being released, Rodgers got a knock at the door.
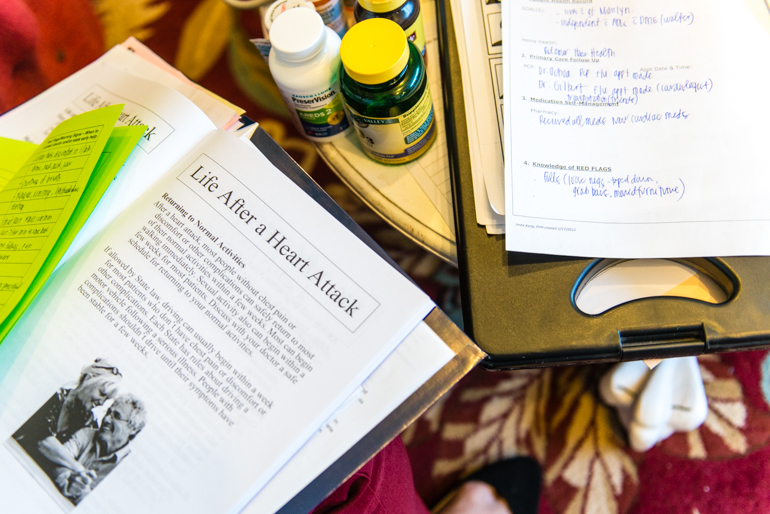
Nurse Tiffanie Abrajano and social worker Valerie Ellis were there to make sure his transition home had gone smoothly. They checked his medications one by one and made sure he knew how to take them. They walked through the house looking for loose rugs and other obstacles that could cause him to fall again. They also asked about safety bars in the bathrooms, and whether he needed a caregiver to help with bathing and dressing.
“We are trying to see if there is anything you might need here in your home to potentially keep you from going to the hospital,” Ellis said. “Do you feel like you have enough assistance?”
“I think I do,” said Rodgers, who lives with a friend. “I feel much stronger… And if I need any help, I can get it.”
For elderly patients like Rodgers, leaving the hospital is fraught with risk. Most are sent home or to nursing facilities after just a few days, still reeling from acute illnesses — not to mention the chronic conditions they are also confronting.
“Just because they have had four days in a hospital doesn’t mean they are better,” said Mary Naylor, a gerontology professor at the University of Pennsylvania School of Nursing.
It’s during that critical time when problems can occur. Patients may get sicker because they don’t have access to medications, transportation, food or crucial equipment such as oxygen tanks. And many don’t have relatives or caregivers to help with the daily tasks that they were able to perform unassisted before being hospitalized.
“There are gaps in care, there are gaps in communication, there are gaps in adequate preparation for patients and families,” said Naylor, who designed a transitions model to address these problems.
In recent years, federal health officials have begun penalizing hospitals for high rates of readmission and sponsoring pilot projects — like the one that sent a social worker and nurse to see Rodgers — to help ensure smoother discharges.
Hospitals and community groups are experimenting with different methods to improve the transition of elderly patients from the hospital.

Some of them seek to strengthen communication with primary care doctors, or use technology to track patients across different health systems. Others emphasize closer partnerships between hospitals and community groups that provide meal delivery, transportation and other social services.
A program developed at the University of Colorado, for example, follows patients for the first month after their discharge, helping them manage their medications, schedule follow-up appointments and recognize signs of trouble.
San Diego County received a federal grant to improve handoffs from the hospital using an adaptation of the University of Colorado’s program. The county’s Aging and Independence Services agency partnered with four hospital systems — Scripps Health; University of California, San Diego; Palomar Health, and Sharp HealthCare — to serve more than 50,000 Medicare beneficiaries at the highest risk of medical complications after discharge.
The efforts aim to improve care and save money. Poorly managed transitions can waste medical services and increase health care costs. The federal government has estimated that nearly 20 percent of Medicare patients return to the hospital within 30 days, costing more than $26 billion annually.
The penalties and programs around the country are starting to make a dent in the problems associated with poorly handled discharges, experts said. The San Diego County program saved Medicare an estimated $13.8 million over a two-year period between 2013 and 2015, primarily because of reduced hospital readmissions.


But experts are quick to note that more needs to be done. Naylor said providers can’t stop looking after patients just a month after they are discharged. “It’s not just thinking about today or tomorrow or the next 30 days,” she said. “For chronically ill, older people, what is their long-term trajectory?”
Programs like the one in San Diego County aren’t a panacea. It serves only a portion of Medicare beneficiaries, and people aren’t eligible for the help while they are in a nursing facility.
John Statler, 88, for example, returned to the emergency room at Palomar Hospital three times within the first week of his discharge to a nursing home. Statler had spent several days at the hospital after a fall left him with a severe head wound. His daughter said the hospital saved his life but didn’t then ensure that he had what he needed to recover after being discharged. In the end, he had to be readmitted.
Transition difficulties often start for elderly patients when they’re preparing to be discharged from the hospital. That’s when medical staffers quickly read a list of instructions to patients and hand them new prescriptions. Older patients may not understand what they are being told because they have dementia or are weakened and confused from their time in the hospital. Some are simply anxious to leave and not paying close attention.
“You are trying to reach them and do that education at such a critical time, but they are nowhere near cognitively ready to receive that,” said Joe Parker, lead nurse of care transitions at Palomar Health. “And we don’t have the luxury of time to wait.”
Back at home, family members and caregivers are often asked to take on medical tasks that would make “most first-year RNs shake in their boots,” said Robyn Golden, director of health and aging at Rush University Medical Center in Chicago. That can lead to medication mix-ups, infections and other problems — especially since the average hospital stay has shrunk.
“People are going home sicker, quicker and they are not returning to their prior selves as quickly – if at all,” Golden said.

Nurse Patrice Gadd visits Joseph Taylor, 88, at Palomar Hospital in March. Gadd informs Taylor that he’ll get a home visit and a month of follow-up to help keep him out of the hospital. (Heidi de Marco/KHN)
Adding to the potential complications is the fact that primary care doctors are often unaware their elderly patients are in the hospital, so they can’t step in to ensure treatment plans are followed.
The main issue the San Diego program is designed to address is the disconnect between hospitals and social services agencies, which have traditionally operated in separate silos, San Diego County and hospital officials said.
“There is a point where the hospital can’t do any more” for patients who have been discharged, said Cecile Davis, coordinator of the remote patient monitoring for Sharp HealthCare. “The key is to know when to turn them over to the community.”
To figure out what patients like Alton Rodgers need, nurses and social workers ask critical questions, said Carol Castillon, who manages the care transitions program for the county.
Do they have transportation to get to the doctor? Do they understand their medications? Do they need an in-home caregiver?
The over-arching question, Castillon said, is: “What are the long-term services we can bring in so that this person isn’t coming back to the hospital?”

Taylor works with physical therapist Jules Stewart. (Heidi de Marco/KHN)
Castillon said that before starting the project with the hospitals, the county regularly found older people in their homes who had been recently discharged and were unable to care for themselves. “They were sick, they were unable to get medications, they didn’t have food,” she said.
Participating hospitals identify patients for the program before they are discharged.
At Palomar Hospital one spring day, nurses Patrice Gadd and Rachel Ricchio stood at the bedside of 88-year-old Joseph Taylor, a former physical therapist who had come to the hospital with pneumonia and was diagnosed with congestive heart failure.
Gadd told him that he could get a home visit and a month of follow-up to help keep him out of the hospital. Taylor and his wife, who had recently moved from Colorado, both agreed that any help would be welcome.
Gadd urged Taylor to call the doctor if he started feeling sick again. “The problem is that the older we get, the less reserves we have in our gas tank,” she said. Things “can go south really, really quickly.”
Nearly three months after his hospitalization, however, Taylor hadn’t returned to the hospital.
This story was reported while its author, Anna Gorman, participated in a fellowship supported by New America Media, the Gerontological Society of America and The Commonwealth Fund.
KHN’s coverage of aging and long-term care issues is supported by a grant from The SCAN Foundation, and its coverage of late life and geriatric care is supported by The John A. Hartford Foundation.








