Jean Hanvik decided that enough was enough. When a painful intestinal inflammation flared in 2014, the 55-year-old benefits communications consultant balked at her doctor’s recommendation that she undergo another abdominal CT scan — her fourth in eight years.
“I’d just read about how abdominal CTs are one of the highest-risk tests [in terms of radiation exposure] and should not be repeated unless there was a major change,” said Hanvik, who lives in Minneapolis. In the past, antibiotics and a bland diet had quelled her recurrent diverticulitis. Hanvik said she wanted to follow that approach again but avoid a scan, which contains about 10 millisieverts (mSv) of radiation, the rough equivalent of 200 chest X-rays or 1,500 dental X-rays.
“I don’t think she appreciated my uncharacteristic behavior,” said Hanvik, adding that her primary care doctor reluctantly agreed, but made her promise to return within 48 hours if she did not improve. Hanvik got better, as she had previously.
Hanvik’s newfound assertiveness and her questions about the necessity of a CT scan reflect a growing awareness of the potential pitfalls of diagnostic imaging, which in the past two decades has exploded into a $100 billion-a-year business.
Imaging has aided diagnosis and helped many patients avoid exploratory surgery, but it has also spawned concerns about misuse. Experts cite ballooning costs, including from duplicate procedures, potential harm from the tests themselves and the overtreatment of harmless conditions found during scans. These “incidentalomas” — so named because they are found unexpectedly — include benign lung and thyroid nodules and other common conditions that can lead to unnecessary and expensive workups as well as treatment that can cause complications.
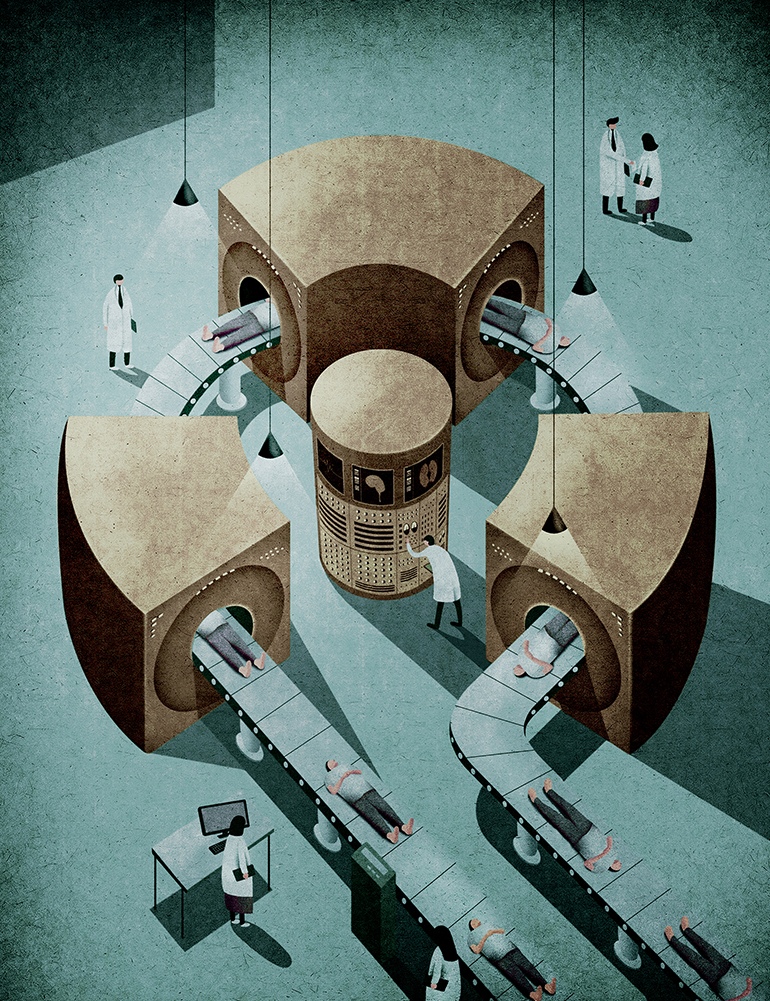
(Illustration by Kai Ti Hsu for The Washington Post)
Much of the attention has focused on computed tomography, or CT, scans, which use hundreds of X-rays to create detailed three-dimensional images that enable doctors to see things previously visible only through a biopsy or surgery.
Like X-rays and PET scans, CT scans use ionizing radiation, which can damage DNA and cause cancer. Two other imaging technologies, MRI scans and ultrasound, do not use radiation. CTs are used for a plethora of reasons, among them finding kidney stones, evaluating chest pain and detecting tumors or other abnormalities.
Widely hailed as one of the most important medical advances of the past century, CT scans were developed in the 1970s. Their use in the United States grew from 3 million in 1980 to more than 85 million in 2011. Although CT scans are an essential diagnostic tool, the Food and Drug Administration reports that an estimated 30 to 50 percent of imaging tests are believed to be medically unnecessary.
“We have this view that we only really use imaging when it’s really necessary,” which is no longer the case, said Rebecca Smith-Bindman, a professor of radiology, epidemiology and obstetrics and gynecology at the University of California, San Francisco. “The truth is, now it’s ubiquitous. And many of these tests don’t need to be done.”
Like X-rays, CT scans represent a potentially significant health problem, one that experts say may not show up for years: cancer caused by radiation. In most cases, it is impossible to definitively attribute cancer to radiation exposure that occurred years or even decades earlier. And overall, the risk from a single scan is small: The National Cancer Institute (NCI) estimates that the additional risk of developing a fatal cancer from a scan is 1 in 2,000, while the lifetime risk of dying of cancer is 1 in 5.
The question of risk remains a matter of fierce debate among radiologists: Some say that the amount of radiation used in diagnostic studies is safe and that the benefits far outweigh the small chance that a person will develop cancer. But other experts, including Smith-Bindman, say that while patients should never avoid scans that are medically necessary, excessive radiation doses and indiscriminate use of imaging pose a clear and demonstrable danger.
Studies published in 2007 and 2009 by teams from Columbia University and the NCI predicted that up to 2 percent of future cancers — about 29,000 cases and 15,000 deaths annually — might be caused by CT scans. A 2011 report by the Institute of Medicine found that the two environmental factors most strongly associated with breast cancer were radiation exposure and the use of post-menopausal hormones.
While a single scan would rarely be concerning, many Americans undergo multiple tests. A 2009 study by researchers at Brigham and Women’s Hospital in Boston found that among 31,000 patients who had a diagnostic CT scan in 2007, 33 percent had more than five during their lifetime, 5 percent received 22 or more, and 1 percent underwent more than 38 scans.
From Necessity To Overuse
Some hospitals tend to perform double scans — one with a contrast agent and a second without it. Doctors sometimes refuse to accept or are unable to access radiology studies done elsewhere and send patients for duplicate tests at a facility in which they have an ownership interest. Doctors who have a financial stake in radiology clinics or who own scanners use imaging substantially more often than those who don’t, studies have found. And increasingly, specialists are requiring that patients get a scan before they first see a patient.
According to the FDA, which has launched an initiative to reduce unnecessary exposure to medical radiation, the effective doses from diagnostic CTs are “not much less than the lowest doses of 5 to 20 mSv received by some of the Japanese survivors of the atomic bombs” dropped over Hiroshima and Nagasaki in 1945. Some of these survivors have “demonstrated a small but increased radiation-related excess relative risk for cancer mortality.”
Radiation exposure is cumulative, and children, who undergo between 5 million and 9 million CT scans annually, are much more vulnerable to its effects.
Concerns about overuse and potential harm have prompted actions by federal health officials as well as consumer and physician groups. These include the Image Wisely and Image Gently campaigns, as well as the national Choosing Wisely effort, which seeks to educate patients and doctors about unnecessary tests such as CT scans for headaches or back pain.
A “decision support” system that creates a set of standards for doctors to follow, pioneered at Massachusetts General Hospital in Boston, reduced the rate of inappropriate imaging tests from 6 percent in 2006 to 1.5 percent in 2014, said James Brink, the hospital’s radiologist-in-chief. A similar statewide program in Minnesota cut the growth rate from 7 percent per year to about 1 percent annually.
New Medicare rules will require doctors to consider appropriateness criteria developed by the American College of Radiology when ordering imaging. Beginning this year, Medicare will reduce by 5 percent reimbursement for CT scans performed on machines that fail to meet modern standards, including the ability to automatically adjust radiation doses.
But significantly reducing the number of unnecessary CT scans may be an uphill battle.
A recent study found that doctors who order a lot of tests — a practice known as defensive medicine — get sued less often.
Some radiologists say they spend their days reading scans that trigger a cascade of follow-up tests and procedures for conditions that nearly always turn out to be benign. “I see two or three [incidentalomas] on every scan,” said Jill Wruble, a radiologist at the VA Medical Center in West Haven, Connecticut, who teaches at the Yale School of Medicine. “I never see a normal patient.”
Financial incentives also fuel the casual use of scans. “Radiology has become an enormous profit” center for hospitals, Smith-Bindman said. “The amount we get paid is very high” under fee-for-service systems.
Patient demand is a key factor. Many people, unaware of the radiation risk, push for tests in the erroneous belief that they signify cutting-edge care. “If a patient requests [a CT scan] and a doctor says no, it could be a good starting point for a conversation,” said Orly Avitzur, medical director for Consumer Reports. But too often, doctors feel pressed for time so they just order the test. “As a practicing neurologist, I can tell you it is a very tough thing to say, ‘No, this is not needed at this time.’ ”
To determine whether a CT is necessary, Avitzur said, patients should ask why the scan is being done, how the results might affect treatment and whether an alternative such as ultrasound or an MRI could be used instead.
How Much Is Too Much?
Among radiologists, the debate about the risk of cancer from diagnostic CTs rages.
“Everything we do in medicine involves trade-offs,” said Smith-Bindman, who directs UCSF’s Radiology Outcomes Research Lab. “The risks of radiation are real, and radiation leads to cancer. I think the data are quite compelling and not that hard to understand.”
But others disagree. “I don’t think the risks are as clear-cut” as Smith-Bindman contends, said Mass General’s Brink, vice chairman of the board of the American College of Radiology. In a recent article he co-authored, Brink characterized the risk of cancer from diagnostic scans as “unproved” and “overemphasized,” based in part on uncertainty about the effect of radiation.
Scott Berger, director of neuroradiology at the Mount Kisco Medical Group in New York, agrees. “The risk of dying from a cancer that is not detected is thousands of times greater than” from radiation, he said. “These tests are lifesaving, they are great for patients.”
But Marta Hernanz-Schulman, medical director of radiology at the Monroe Carell Jr. Children’s Hospital at Vanderbilt in Nashville, is less gung-ho.
“Is radiation a real problem?” she asked. “We don’t know, but we need to act as if it were.” Studies performed in the United Kingdom in 2012 and Australia in 2013 found an increase in cases of leukemia and malignant brain tumors among children and young adults who had undergone CT scans. One concern, said Hernanz-Schulman, a past president of the Society for Pediatric Radiology, is that many children undergo CT scans in adult facilities and may receive excessive doses because scanners are not adjusted between patients.
At Vanderbilt, children brought to the ER after a motor vehicle accident used to automatically get an abdominal CT scan. “Now we get liver enzymes first to see if they have a liver [injury] and we need a CT scan,” she said. In the past decade the number of CT scans has been cut by nearly half, she said.
Smith-Bindman said that excessively high radiation dosage is a problem requiring urgent attention. A 2009 study she led found that the actual radiation doses from CT scans varied as much as 13-fold for the same test performed at the same hospital, and these doses were much higher than those required to make a diagnosis. Except for mammography, there are no federal regulations governing radiation doses.
There are several reasons for the variation, Smith-Bindman said, including the failure to adjust the radiation dose based on body size and a desire to achieve more finely detailed images, which can be achieved by ramping up the dose. Nor are there national standards for technologists who administer CT scans, which involve increasingly sophisticated equipment. Some states don’t even require that they be licensed, allowing virtually anyone to operate the equipment.
“There’s no standardization of how these exams get conducted,” Smith-Bindman said. “There’s no oversight and no one’s responsible for this.”
Recently, she said, she spoke to a group of 300 radiology technologists and was “dumbfounded” by their questions. One asked her, “How do I pick a dose?” The technologist said she had devised her facility’s CT protocol, a job that is supposed to be performed by radiologists. Another said that in her hospital, “no one cares” about radiation doses.
Test Declined
Although Jean Hanvik avoided an abdominal CT after her diverticulitis flared, a few months later she had a different experience with a painful wrist. Before an orthopedist would see her, he required that she get an MRI scan, much of which she had to pay for out of pocket. It revealed that she had arthritis. Hanvik wonders why an expensive scan was necessary, particularly before ever talking to the doctor.
“I’m frustrated that diagnostic imaging has become the first line of defense,” she said. “I’m learning to ask a lot more questions.”