While Congress continues to struggle with how to “repeal and replace” the Affordable Care Act, the Trump administration today unveiled its first regulation aimed at keeping insurers participating in the individual market in 2018.
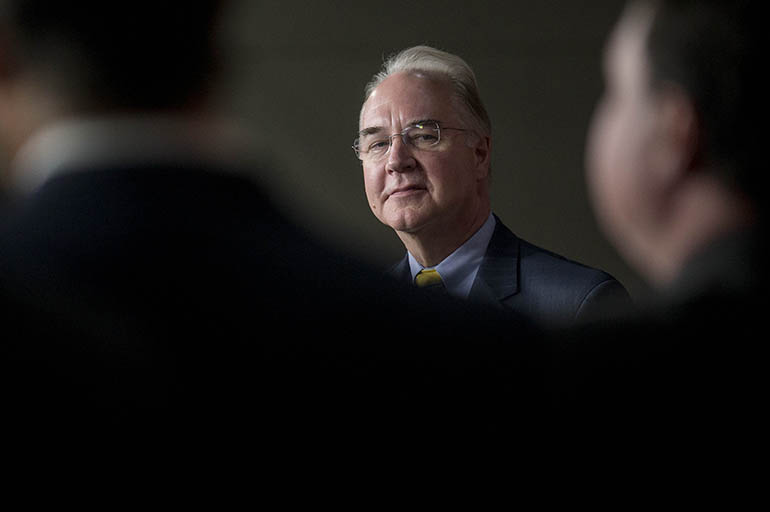
“These are initial steps in advance of a broader effort to reverse the harmful effects of Obamacare, promote positive solutions to improve access to quality, affordable care and ensure we have a health system that best serves the needs of all Americans,” Tom Price, secretary of the Department of Health and Human Services said in a Twitter message.
But the new rule, which had been widely expected, was actually begun by the outgoing Obama administration. In part, it is an effort to address complaints by insurers that consumers were “gaming” the system to purchase coverage only when they were sick and then dropping it when they were healthy.
To combat that, the regulation makes it harder for patients to sign up outside of annual open enrollment periods and would allow insurers to collect past-due premiums before starting coverage for a new year. It would also shorten the annual enrollment period by half, from three months to 45 days, ending right between Thanksgiving and Christmas. And it would give insurers more flexibility in the types of plans they offer and return regulation of the size and adequacy of health care provider networks to the states.
But it remains unclear whether the action will be too little, too late to ensure insurance is available next year. That would be necessary to keep congressional Republicans’ promises that people “do not get the rug pulled out from under them” during the transition to a new program, as House Speaker Paul Ryan (R-Wis.) says frequently.
On Tuesday, Humana announced it would stop selling policies in the health exchanges at the end of this year, and on Wednesday Mark Bertolini, the CEO of Aetna, suggested his firm might follow suit, repeating GOP charges that the individual market exchanges are in a “death spiral” where only sick people buy coverage.
While Humana was not a major player in the state exchange market — it only sold policies in 11 states for 2017 — its exit could leave at least 16 counties in Tennessee, including Knoxville, with no insurance company offering policies on the health exchange, according to data from the Kaiser Family Foundation. (KHN is an editorially independent program of the foundation.)
That alarmed Sen. Lamar Alexander (R-Tenn.), chairman of the Senate Health, Education, Labor and Pensions Committee, who has been one of the leading voices in Congress advocating a slower repeal and replace strategy.
“Yesterday’s news from Humana should light a fire under every member of Congress to work together to rescue Americans trapped in the failing Obamacare exchanges before they have no insurance options next year,” Alexander said in a statement.
Last year Aetna’s Bertolini also cited losses in the market as the reason for the company’s scaling back participation in the exchanges, although in an unrelated case, a judge’s ruling later said the decision had at least as much to do with pushing federal officials to allow Aetna to merge with Humana. On Monday that merger was officially called off after being blocked by a judge.
The new rules were greeted with cautious optimism by insurance industry trade groups.
“While we are reviewing the details, we support solutions that address key challenges in the individual market, promote affordability for consumers, and give states and the private sector additional flexibility to meet the needs of consumers,” Marilyn Tavenner, president and CEO of America’s Health Insurance Plans, said in a statement.
The Alliance of Community Health Plans, which represents nonprofit insurers, called the regulation “a promising first step.” But in a statement, president and CEO Ceci Connolly warned that the rule “does not resolve all of the uncertainty for plans and patients alike. Without adequate funding it will be extremely difficult to provide high-quality, affordable coverage and care to millions of Americans.”
Groups representing patients, however, were less happy with the changes. They argue that the rules could result in higher out-of-pocket costs.
Ron Pollack, executive director of the consumer group Families USA, said the new administration “is deliberately trying to sabotage the Affordable Care Act, especially by making it much more difficult for people to enroll in coverage.”
Sick people are likely to jump through any hoops required to get coverage, but healthy people are less inclined to sign up when it is more difficult. So by making it harder for healthy people to enroll, said Pollack, “they are creating their own death spiral that would deter young adults from gaining coverage, thereby driving up costs for everyone.”
And the American Cancer Society said that the new rules could hurt cancer patients in particular — for example, when they need to purchase new coverage after becoming too sick to work or moving to be closer to health providers. The proposed changes “would require documentation that is often challenging to quickly obtain,” and could “delay a patient’s treatment and jeopardize a person’s chance of survival,” said a statement from Chris Hansen, president of the society’s Cancer Action Network.
Unless the new administration changes the date, insurers must decide by May 3 if and where they will sell insurance for next year on the state exchanges.
Meanwhile, the Republican-led Congress remains in a deadlock between conservatives in the House, who want to repeal the health law as soon as possible, and moderates in the Senate like Alexander, who want to wait until there is agreement on what will replace it.
“We should just do what we said we would do,” Rep. Raul Labrador (R-Idaho) told reporters on Tuesday.
Conservatives say, at a minimum, Congress should pass the partial repeal bill it passed in 2015 that President Barack Obama vetoed. That measure would eliminate the expansion of the Medicaid program, financial help for people to purchase insurance, the penalties for not having coverage, and all the taxes that pay for the program, among other things.
“Why would it be difficult to get [the Senate] to vote for something they already voted for?” asked Rep. Mark Meadows (R-N.C.).
But congressional budget scorekeepers in January said that bill, which has no replacement provisions, could result in a doubling of premiums and 32 million more people without insurance.
And Republicans in the Senate, as well as President Donald Trump, continue to say that repeal and replace should take place simultaneously.
“I thought we were embarked on an effort to replace it,” said Sen. John McCain (R-Ariz.).