When Greta Christina fell into a deep depression five years ago, she called up her therapist in San Francisco. She’d had a great connection with the provider when she needed therapy in the past. She was delighted to learn that he was now “in network” with her insurance company, meaning she wouldn’t have to pay out-of-pocket anymore to see him.
But her excitement was short-lived. Over time, Christina’s appointments with the therapist went from every two weeks, to every four weeks, to every five or six.
“To tell somebody with serious, chronic, disabling depression that they can only see their therapist every five or six weeks is like telling somebody with a broken leg that they can only see their physical therapist every five or six weeks,” she said. “It’s not enough. It’s not even close to enough.”
Then, this summer, Christina was diagnosed with breast cancer. Everything related to her cancer care — her mammogram, biopsy, surgery appointments — happened promptly (like a “well-oiled machine,” she said), while her depression care stumbled along.
“It is a hot mess,” she said. “I need to be in therapy — I have cancer! And still nothing has changed.”
A new law signed by Gov. Gavin Newsom in October aims to fix this problem for Californians. Senate Bill 221, which passed the state legislature with a nearly unanimous vote, requires health insurers across the state to reduce wait times for mental health care to no more than 10 business days. Six other states — including Colorado, Maryland and Texas — have similar laws limiting wait times.
Long waits for mental health treatment are a nationwide problem, with reports of patients waiting an average of five or six weeks for care in community clinics, at Department of Veterans Affairs facilities and in private offices from Maryland to Los Angeles County. Across California, half of residents surveyed by the California Health Care Foundation in late 2019 said they had to wait too long to see a mental health care provider when they needed one.
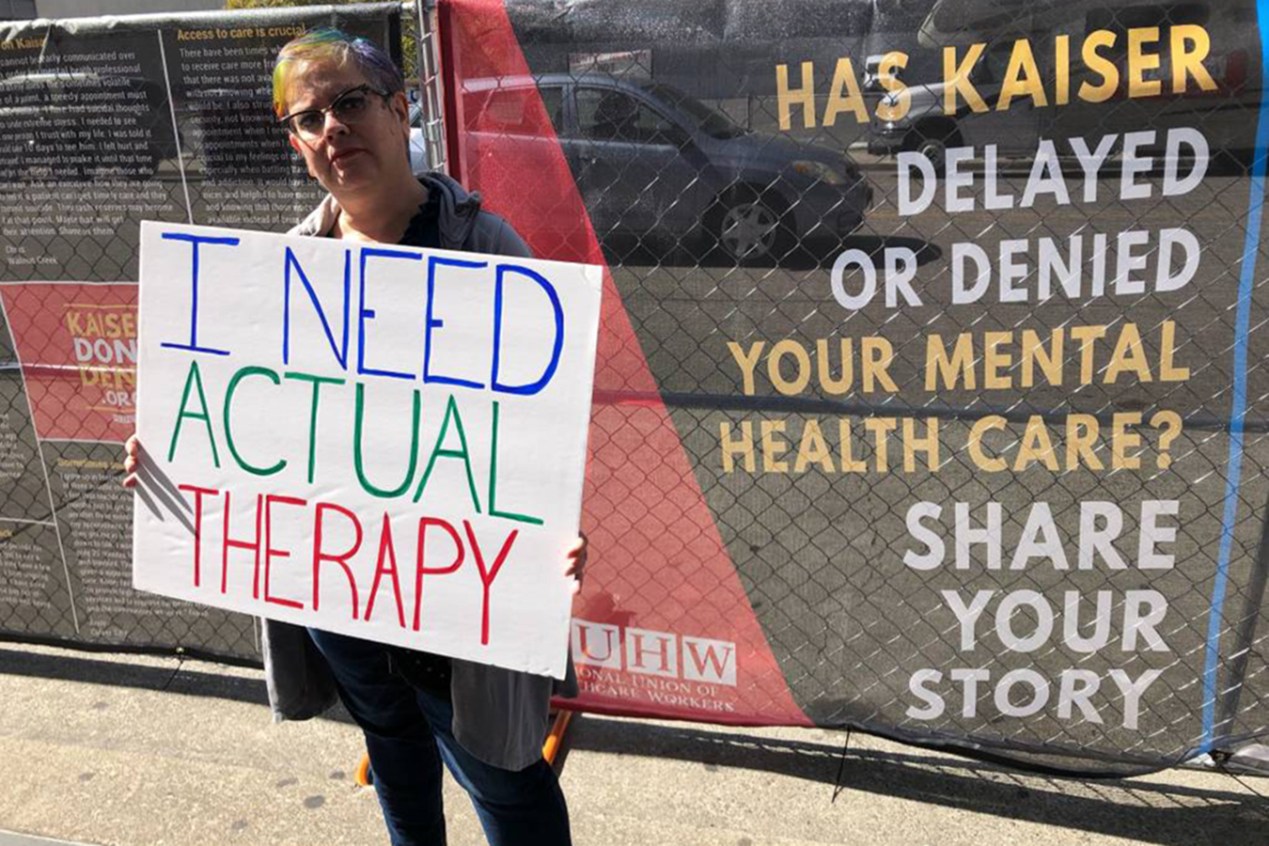
At Kaiser Permanente, the state’s largest insurance company, 87% of therapists said weekly appointments were not available to patients who needed them, according to a 2020 survey by the National Union of Healthcare Workers, which represents KP therapists — and was the main sponsor of the California wait times legislation.
“It just feels so unethical,” said triage therapist Brandi Plumley, referring to the typical two-month wait time she sees at Kaiser Permanente’s mental health clinic in Vallejo, east of San Francisco.
Every day, she takes multiple crisis calls from patients who have therapists assigned to them but can’t get in to see them, she said, describing the providers’ caseloads as “enormous.”
“It’s heartbreaking. And it eats on me day after day after day,” Plumley said. “What Kaiser simply needs to do is hire more clinicians.”
Kaiser Permanente says there just aren’t enough therapists out there to hire. KP is an integrated system — it is a health provider and insurance company under one umbrella — and has struggled to fill 300 job vacancies in clinical behavioral health, according to a statement from Yener Balan, the insurer’s Northern California vice president of behavioral health.
Hiring more clinicians won’t solve the problem, said Balan, who suggested that sustaining one-on-one therapy for all who want it in the future wouldn’t be possible in the current system: “We all must reimagine our approach to the existing national model of care.”
Kaiser Permanente lodged concerns about the wait times bill when it was introduced. And the trade group representing insurers in the state, the California Association of Health Plans, opposed it, saying the shortage of therapists would make meeting the two-week mandate too difficult.
“The COVID-19 pandemic has only exacerbated this workforce shortage, and demand for these services significantly increased,” said Jedd Hampton, a lobbyist for the California Association of Health Plans, in testimony during a state Senate hearing for the bill in the spring.
Hampton referred to a University of California-San Francisco study that predicted California would have nearly 30% fewer therapists than needed to meet demand by 2028.
“Simply put, mandating increased frequency of appointments without addressing the underlying workforce shortage will not lead to increased quality of care,” Hampton said.
Lawmakers pushed back. State Sen. Scott Wiener (D-San Francisco), who authored the bill, accused insurers of overstating the shortage. State Sen. Connie Leyva (D-Chino) said that the therapeutic providers are out there but that insurers are responsible for recruiting them into their networks by paying higher rates and reducing administrative burdens.
If insurers want more young people to enter the mental health care profession, they must improve salaries and working conditions now, said state Sen. Richard Pan (D-Sacramento). (A 2016 KQED investigation uncovered multiple ways that insurers save money by keeping provider networks artificially small.)
As bipartisan support for the bill grew in Sacramento, insurers withdrew their formal opposition.
But whether other states have the political will, or the resources, to legislate a similar solution is unclear, said Hemi Tewarson, executive director of the nonpartisan National Academy for State Health Policy in Washington, D.C. Although California may be able to force insurers to hire more therapists, she said, places like New Mexico, Montana, Wyoming, and parts of the South don’t have enough therapists at any price.
“They don’t have the providers, so you could fine the insurers as much as you want, you’re not going to be able to, in the short term, make up those wait times if they already exist,” she said.
The new California law is a solid step toward improving access to mental health care, with communities of color standing to benefit the most, said Lonnie Snowden, a professor of health policy and management at the University of California-Berkeley. African Americans, Asian Americans and Latinos face the most barriers getting into care, Snowden said, and when people of color do come in for treatment, they are more likely to drop out.
Oversight and enforcement are needed for the new rules to work, said Keith Humphreys, a psychiatry professor at Stanford University. Kaiser Permanente has data systems that can track the time between appointments, but other insurers set up contracts with therapists in private practice, who manage their own caseloads and schedules.
”Who would keep track of whether people who’ve been seen once were seen again in 10 days, when it’s hard enough just to keep track of how many providers we have and who they are seeing?” he asked.
Questions like that one will fall to state regulators, primarily the California Department of Managed Health Care. The department has fined insurers $6.9 million since 2013 for violating state standards, including a $4 million penalty against Kaiser Permanente for excessive wait times for mental health care. Previous state law required insurers to provide initial mental health care appointments within 10 days, and the new law clarifies that they must do the same for follow-up appointments.
Greta Christina, who gets her care at a Kaiser Permanente facility, said she is desperate for the new law to start working. It takes effect on July 1, 2022. Christina thought about paying out-of-pocket in the meantime, to find a therapist she could see more often. But in a cancer crisis, she said, starting over with someone new would be too hard. So she’s waiting.
“Knowing that this bill is on the horizon has been helping me hang on,” she said.
This story is part of a partnership that includes KQED, NPR and KHN.